Infection prevention is a shared responsibility—spanning from clinical teams to EVS professionals to the products and processes we trust to keep environments safe. In Contec Professional’s recent webinar, industry experts gathered to explore the science and strategy behind disinfection in healthcare settings, with practical demonstrations, key regulatory insights, and candid discussions about real-world challenges.
If you missed it, don’t worry—we’ve distilled the major takeaways into this blog post to help you optimize disinfection practices across your facility.
Understanding Disinfection: What It Is—and What It Isn’t
Dr. Mark Wiencek, the Principal Microbiologist with Contec’s Technical Services Group, kicked off the webinar by demystifying disinfection:
“You can’t see microbes, and you can’t see them dying—but you can gain confidence that disinfection is occurring with the right processes, products, and partners.”
Disinfection, at its core, is about reducing large populations of harmful microbes on inanimate surfaces. But it’s not just about applying a chemical and walking away—it’s about choosing EPA-registered disinfectants, understanding their active ingredients, knowing their wet contact times, and pairing them with compatible tools to avoid degradation.
Key Factors for Effective Disinfection
1. EPA Registration and Label Claims
The EPA regulates disinfectants as pesticides under the FIFRA Act, ensuring that each product is both safe for humans and effective against specific microbes when used as directed. Labels matter—especially when it comes to:
- Wet contact time
- Target pathogens
- Shelf life and expiration
- Approved dilutions
2. Dilution: Precision Over “Glug Glug”
Concentrated disinfectants are widely used in EVS due to cost efficiency and storage advantages. But dilution must be exact—too much dilution weakens efficacy; not enough dilution can harm surfaces, staff, or patients.
Dr. Wiencek emphasized:
“You’ve got two dials—concentration and wet contact time. Get those right, and you’ve got a fighting chance against harmful microbes.”
Dispensing systems must be regularly tested and maintained. A recent study published in Infection Control & Hospital Epidemiology revealed that over 50% of the use dilutions from dispensing events in 10 hospitals were outside their labeled concentrations, compromising performance.
3. Tools Matter: How Wipes and Mops Affect Efficacy
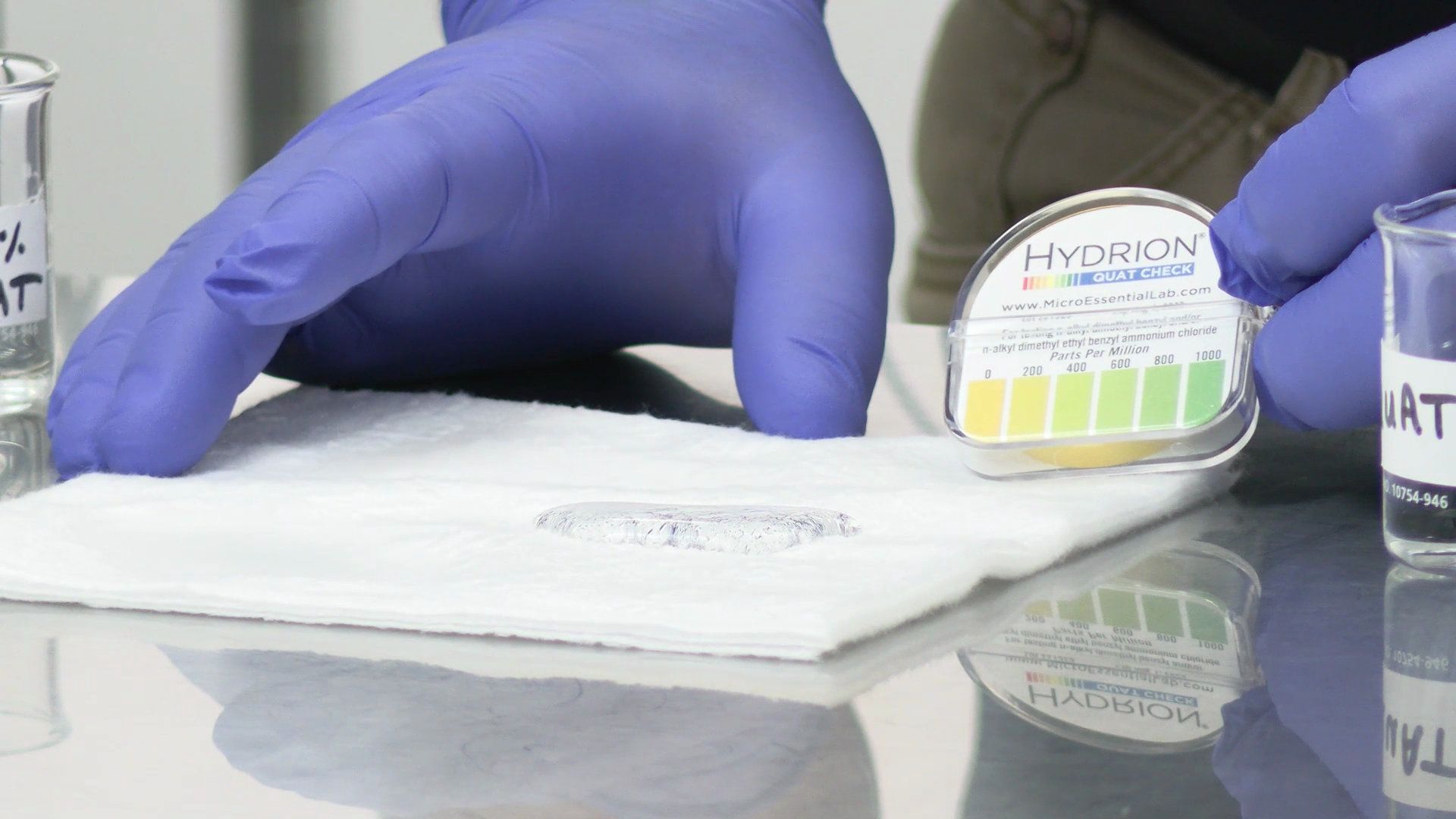
A highlight of the webinar included a live demo by Ron Sample, a former EVS director and now Contec Professional’s Executive Technical Support Specialist. Using test strips and different types of applicators, he demonstrated how laundered microfiber towels or imcompatible disposable wipers can bind quaternary ammonium compounds (quats)—the most common active ingredient in hospital-grade disinfectants.
 ContecClean Cloth stood out as a single-use, disposable wiper that ensures consistent delivery of disinfectant—without quat binding. This product also exhibits a unique feature – it will not absorb water alone. The water must contain at least some disinfectant to break the surface tension and be absorbed into the wiper.
ContecClean Cloth stood out as a single-use, disposable wiper that ensures consistent delivery of disinfectant—without quat binding. This product also exhibits a unique feature – it will not absorb water alone. The water must contain at least some disinfectant to break the surface tension and be absorbed into the wiper.
👉Key Insight: If your wipes reject liquid or don’t absorb evenly, your disinfectant may be ineffective— or missing entirely.
4. Why Clinical and EVS Teams Must Work Together
Michelle Knight, an experienced Infection Preventionist, emphasized collaboration:
“EVS and IP should be partners in every decision around disinfection—from chemistry to application tools—because our collective goal is patient and staff safety.”
High turnover areas like ORs or L&D often demand faster dwell times, while other departments may prioritize products with low residues. There’s no one-size-fits-all solution, and flexibility is key.
5. Watch-Outs and Best Practices
Avoid These Common Pitfalls:
- Leaving lids open on pre-saturated wipes (dry wipes = no disinfection)
- Using incompatible textiles (causes quat binding or chemical degradation)
- Mixing up different solutions in wall dispensers or improper dilutions
- Overlooking test strip expiration dates
- Assuming one process fits every department
Best Practices:
- Spot-test use dilutions regularly using compatible test strips
- Train staff on product-specific instructions (e.g., shake strip, wait 15 sec on strips)
- Use visual indicators (like how wipes absorb) as early warning signs
- Prioritize tools that maintain chemical stability
- Clean and disinfect tools (not just surfaces) to avoid biofilm
Special Focus: Combatting MDROs in Acute and Long-Term Care
Multidrug-resistant organisms (MDROs) pose a persistent threat, particularly in long-term care settings, where patients may have long-term medical devices or immune vulnerabilities. Michelle Knight reminded us:
“You can pour a disinfectant on a surface, but if you don’t maintain contact time or wipe correctly, you’ve done nothing.”
Both process and product are critical. Facilities should invest in effective disinfectants—and in training their teams to use them correctly.
Final Takeaway: Disinfection is a System, Not a Step
The webinar wrapped with a powerful message: disinfection is not just a product—it’s a system of chemistry, process, education, and teamwork.
“If the wipes are dry, the germs don’t die.”
— Dr. Mark Wiencek
From choosing the right chemistry to monitoring dilution accuracy to using compatible tools, every component matters. Contec Professional is committed to helping healthcare providers build disinfection systems that work—for patients, staff, and the environments we all share.
Want to Learn More?
👉 Watch the full webinar on demand here
Contact Contec Professional to schedule a product consultation or technical training session for your team.



.png)